|
The Canadian Conference of Catholic Bishops, the Pontifical Academy for Life, and other key partners are organizing an international interfaith symposium on palliative care. Entitled “Towards a Narrative of Hope”, this symposium will take place on May 21-23, 2024, in Toronto. With the objective to educate and build a culture of social responsibility in palliative care, experts from medical, ethical and pastoral contexts will focus on translating insights from the presentations and discussions into concrete strategies of actions. You can already watch a short video on the purpose of the symposium and the vital role of faith-based organizations and communities in promoting human dignity, compassion, and respect for patients and their families through the illness and dying process. Please find below, for your information the videos announcing this international interfaith symposium on palliative care. Video in French by Bishop Noël Simard, Bishop of Valleyfield QC, and Member of the Pontifical Academy for Life (PAV), and Chairman of the Scientific Board for the Symposium: https://youtu.be/zBYKDGrvDlE?si=bHQYZ51-Ol0cuazQ
0 Comments
Great news! The celebration of Sunday Mass has resumed at three hospitals on the First Sunday of Advent in the City of Calgary. Patients, family members and friends, and hospital staff are now able to avail of this pastoral outreach in the following facilities:
The accelerated adoption of the Euthanasia law in Canada has thrown us into a troubling attack on the sanctity of life. Initially introduced by the Canadian Government to alleviate severe physical suffering, the law is now being suggested as a method to "manage" mental health conditions. Bill C-7, an amendment to the Criminal Code relating to medical assistance in dying (MAiD), proposes expanding eligibility for MAiD by removing the requirement that a person's natural death must be reasonably foreseeable. This could allow individuals not nearing the end of their lives, including those with mental illnesses such as depression, to avail themselves of this provision. Since its adoption, over 31,000 medically assisted suicides have occurred in Canada - a number projected to rise significantly with the planned expansion of the law to include those suffering from mental health conditions. However, mental health illnesses are highly treatable. Symptoms can be managed, and lives can be lived to the fullest. Broadening access to MAiD is not the solution, particularly when our priority should be to choose life over death. We must ensure all efforts are taken to protect the most vulnerable from medically assisted premature death, which can be prevented with adequate treatment and care. We should ensure that those suffering from mental illness are treated medically, not through assisted dying. Conservative MP Ed Fast has brought forward a Private Members Bill C-314 to rescind the government’s decision to expand Canada’s assisted suicide laws. The bill asserts that medical assistance in dying should not apply to persons suffering solely from mental illness. The vote will take place by members of parliament on October 18th. As the CCCB urges all the faithful in their Open Letter in May 2023: “We encourage individual Catholics and their families, faith communities, Catholic healthcare professionals and any other people of good will to continue courageously and unwaveringly to witness to life, to tend to and accompany the sick, to resist pressure to support or participate in ‘MAiD,’ and to pray that our law makers may see the harm in what they are permitting to take place.” Let's continue to pray for those living with mental health challenges and illnesses and those who care for them, that God may strengthen them in hope, and that they may find the support they need from family, healthcare professionals, faith communities, and others. The Catholic Women's League (CWL), a national organization of Catholic women, emphasizes the sanctity of human life as one of their key missions. Amidst the pressing social justice issue of inadequate mental health and palliative care services in Canada, and the critical concern surrounding MAiD, they are urging members and the faithful to take action and reach out to their Member of Parliament, requesting support for Bill C-314. With the vote scheduled for October 18th, time is critical. Please share this vital message with your family and friends.
Notes:
Reading materials:
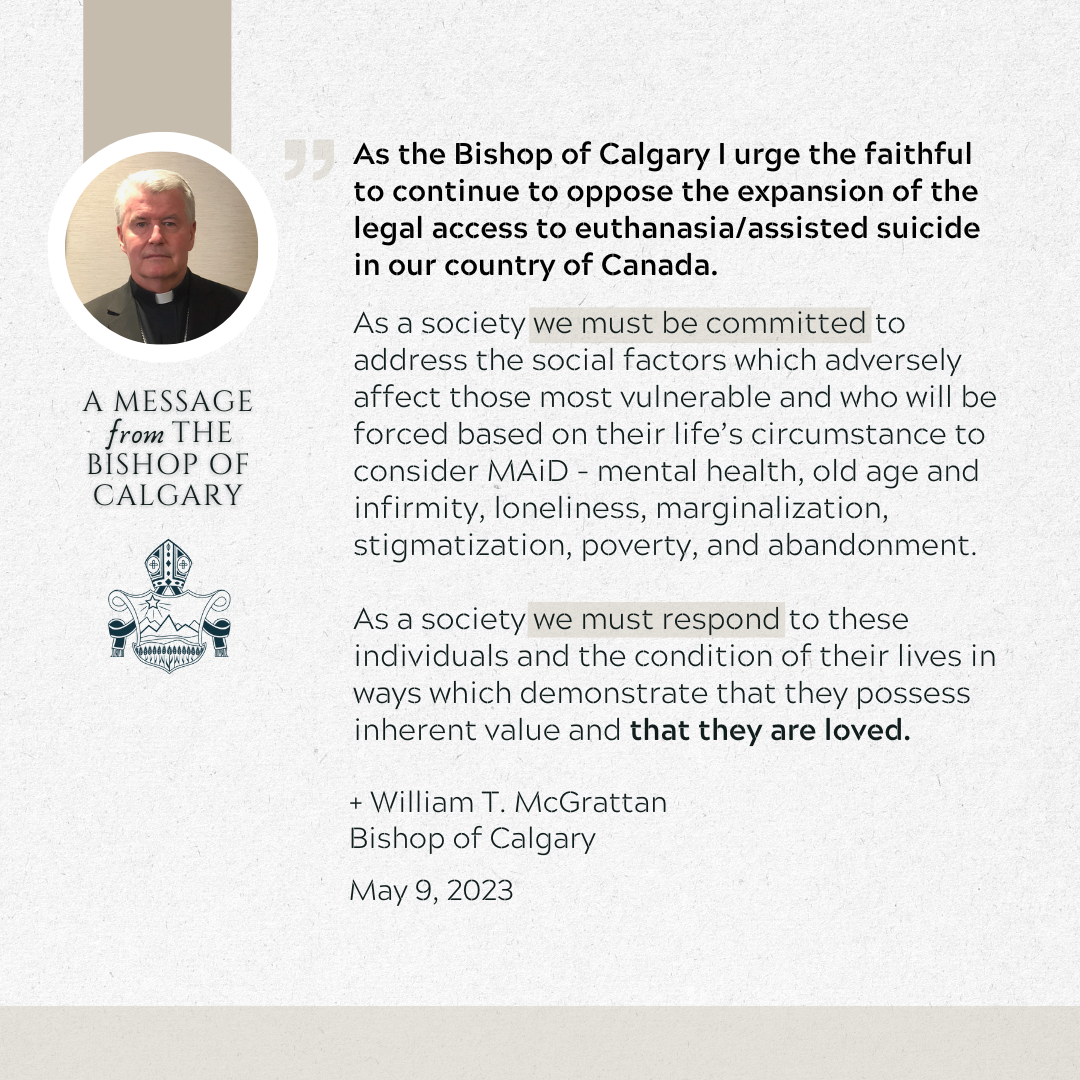
Together with the Canadian Conference of Catholic Bishops (CCCB), Bishop McGrattan is urging the faithful to continue to oppose the expansion of MAiD in Canada. The CCCB has just issued an Open Letter to the Government of Canada and a Message to the Catholic Faithful on May 9 re: Permitting Persons Living with Mental Illness to Access Euthanasia/Assisted Suicide. We ask you to share the Bishop's message with your friends and family:
Let us spend the National Week of Family and Life (NFLW) 2023 united in prayer, reflection, and action, demonstrating our active support for family and life. Indeed, families are “guardians of life” when we love one another within our families and in wider society when we show kindness toward and care for the vulnerable and marginalized.
Note: Day 1 can begin anytime! We want to ensure everybody has the opportunity to join in and take part in this wonderful experience. Don't worry if you missed the start of NFLW, you can join in and start participating in the daily prayers and activities from any day.
Source: National Life & Family Week Daily Prayers & Activities, CCCB, 2023
 Dr. Peggy Thomson-Gibson Dr. Peggy Thomson-Gibson
Canadian Catholics who want a more fulsome public discussion of the law regarding medically-assisted death are being called to use their faith to move a legislative mountain. But take heart. The first item on the change agenda involves something as simple–and important–as writing letters to your Member of Parliament and key government ministers, says Dr. Peggy Thomson-Gibson.
The catch? With people’s lives at stake, there’s no time to lose. A Catholic and Calgary physician, Dr. Thomson-Gibson recently addressed MAiD (Medical Assistance in Dying) at a special meeting held at St. Peter’s parish. There, the medical doctor encouraged Catholics to learn how “we can defend our faith without raising our voices.” To do that, Catholics need solid information about their faith–and about what’s at stake, especially with proposed changes to MAiD law, says Thomson-Gibson. The problem with MAID Approved in 2016, existing MAiD law allows Canadians to choose a medically-assisted death when their death is “reasonably foreseeable.” Health Canada recorded 7,595 MAiD deaths in 2020, up from 1,108 in 2016. For information about why the Church rejects euthanasia or assisted suicide, visit this page. Looking ahead, the number of MAiD deaths to date are a fraction of what was expected had proposed amendments come into effect this March. The now-delayed changes expanded MAiD’s accessibility while simultaneously decreasing oversight, says Dr. Thomson-Gibson. Of primary concern was a change that allowed people with mental illness as their sole criterion to choose a medically-assisted death. People with a severe long-term condition or disability could also access MAiD, opening the door for medically-assisted death to be offered instead of treatment. Opponents say this confuses the notion of a “right” to die with a “duty” to choose death over treatment. This is especially troublesome in a public health system where disabled or mentally-unwell individuals could be made to think they are a financial burden on their families or society. Information released in 2022 shows the proposed changes also cut a mandated reflection period for those whose death is “reasonably foreseeable” under current law. Instead of a 10-day period, the changes required a single day. Another change drops the legal requirement for two witnesses to one and the sole witness could be a paid health professional. These amendments were scheduled to come into effect in March 2023. They were delayed in late 2022, and again last week. This provides more time for study and input. That timeline underscores the opportunity for faith-based outreach, like letters to the Prime Minister and individual Members of Parliament, says Thomson-Gibson. She suggests letter writers model respect in their letters and conversations about MAiD. Catholics looking for more guidance about how “to shed light, not heat” on hot-button topics should check out information from Catholic Voices Canada (https://catholicvoices.ca), adds the doctor.
The World Day of the Sick is celebrated each year on February 11, the liturgical memorial of Our Lady of Lourdes. It is an occasion to pray for individuals who are suffering, and to find concrete ways to draw nearer to them. The Holy Father's 2023 message is entitled: "Take care of him - Compassion as a synodal exercise of healing". In light of the Church's synodal journey, Pope Francis invites us "to reflect on the fact that it is precisely through the experience of fragility and illness that we can learn to walk together according to God's style of closeness, compassion and tenderness."
Pastoral suggestions for the World Day for the Sick (Feb. 11, 2023) for parishes and all the faithful:
Resources for World Day for the Sick:
As human beings with both body and soul, we take good care of ourselves through healthy relationships, especially our relationship with God, and with the help of science. Watch this video and see how both science and the Faith connect.
“Help me!” Out of a dark bathroom in a long term care home, I heard a plaintive cry and froze. I was there to bring the Eucharist, nothing more. I turned to seek out an attendant and heard again, “Don’t leave me!” Heart pounding, I crept forward, identified myself loudly and turned on the lights to find an elderly woman on the toilet. With shaking hands I cleaned her and helped her to stand up. She leaned against me as we washed our hands. Secretly I thought, “I have wiped Christ’s bottom.” Jesus said that whatever we do for the least of his brethren we do for him. This is true whether we cook for our family, give alms to the poor or serve at Mass. However, it might be particularly true when we are called to move out of our comfort zone and give more than we intended to. For example, when we offer to buy a street person a coffee and he chooses a whole meal with it. Or we call to check in on a friend and she spills out her woes for an hour. When we give of ourselves we prefer to have a measure of control over the experience but that is not how God gives of himself. God gave his only son, and Jesus gave his lifeblood for us. God continues to give constantly and completely, so we are called to do the same. This kind of self-emptying service is what Pope Francis called “the art of accompaniment”. “The Church will have to initiate everyone – priests, religious and laity- into this “art of accompaniment” which teaches us to remove our sandals before the sacred ground of the other.” (Evangelii Gaudium 169) I am coming to understand The Art of Accompaniment through a series of talks given by Fr. Tim Boyle at St. Martha’s Parish in Lethbridge . So far Fr. Boyle has noted that accompaniment is not quite the same as caregiving, although it might include that. To accompany someone is to first of all recognize that God is with them. As guest speaker Reno Guimond said, “We are not bringing God to anyone. God has been there long before we show up. We go to see where God is.” Besides recognizing God in each person, we also need to understand how God works in the world. Fr. Boyle encouraged his listeners to imagine God “delighting” in the world as he created it. “God has invested himself in creation,” Fr. Boyle said. “This is not a one-time event but an evolving artwork. If God accompanies us as an artist not as an engineer then God is vulnerable to the unfolding of Creation… God suffers in the process… God chooses to spend himself on creation.” This form of sacrificial support was expressed ultimately by God becoming human and Jesus’ death and resurrection. For us, sacrificial giving of ourselves is often a challenge. Society dictates that one must preserve oneself, must learn to ‘Say No’, and ration one’s time and energy. Yet Creation shows otherwise. Fr. Boyle used the examples of salmon making death runs upstream to spawn, and sunflowers drying up to produce seeds for food and for procreation. “Like salmon and sunflowers, every creature, in order to reach their full potential, needs to empty themselves out”, Fr. Boyle said. So how is this achieved in practical terms? How does one accompany another person, whether continuously or when called upon? It begins when we accept God’s accompaniment of us. This happens through grace which Fr. Boyle suggests is “like manna – something given by God every day which cannot be stored up but only taken advantage of that day.” Grace is not a weapon or superpower, it doesn’t enhance our abilities. Indeed it requires us to first accept that we have no ability without God. We are flawed and vulnerable beings made precious by God’s acceptance. It is God’s grace that sustains us, sanctifies us. When we understand this dynamic we are better prepared to handle the vulnerability of others, to accept it, and handle it gently. Since my first incident of extreme vulnerability in long-term care, my ministry partner and I have been called upon to assist a few others at their times of greatest need, in life and even approaching death. While I still feel my heart pounding each time, the experiences have been deeply humbling. I know God is helping me learn how to cherish the sacred ground of others.
The Calgary Catholic Medical Association (CCMA) would love to invite and meet with you at our upcoming event. Please join us for the White Mass (Feast day of St. Luke) Tuesday, October. 18, 2022 at 7 pm, at St. Mary's Cathedral (Calgary) with Bishop McGrattan. This mass is open to the public and is not limited to only health care professionals. About CCMA The Calgary Catholic Medical Association (CCMA) has been a running lay Association for 20 years. It is the only multidisciplinary Catholic Association of health care providers in Canada. Our mission is to foster the personal and professional formation of healthcare professionals, in accord with the magisterium of the Catholic Church. Membership includes voting and nomination privileges at the AGM, early notification of upcoming events, early bird discount pricing for social events, but most importantly, a community that holds common ground in faith and interest in health care. To share some personal experiences of the CCMA, we have testimonies from a few members of the Executive Council.
I have been part of the CCMA since 2016, first as a spouse of a member, an allied health member, and then as a member of the Board. For me, this association is a place of community and connection with others of the same faith and values. Sometimes religion and spirituality can be very personal and hard to talk about, however, I have realized that spirituality is what gives us meaning in life, whether for ourselves or for the people we care for. This has been the place to share in how we can live out our faith while exhibiting the love and care like Jesus did within both our personal and professional roles. To contact CCMA, visit their website at https://catholicmedyyc.wordpress.com
or email [email protected]
Javier Martinez had just removed his face shield and mask when a woman suddenly appeared in the room and approached him. The woman was a resident of the memory care wing of the seniors’ residence where Martinez was working. She was also positive for COVID-19. “It happened so fast and I remember thinking, ‘it’s highly probable that I’ve got COVID,’” recalls Martinez, a registered nurse and the father of five. He was right. Martinez is a clinical leader in the supportive living section at St. Marguerite Manor, a Covenant Care home in northwest Calgary. Two residents at that facility died in the second wave of the global pandemic declared in 2020. Martinez, however, was infected in Edmonton. He was there in November 2020 to provide support in a seniors’ care home hit much harder by the second wave of the pandemic. In addition to several deaths and widespread infection, many staff at that home were infected and unable to work. While his first test was negative, Martinez developed body aches and a headache soon after his return to Calgary. The nurse knew he had COVID-19 well before the second test yielded a positive result. By then, he and his wife Colette had already discussed what they would do to keep the family safe. They did what they could to keep their kids, ages 13 to three, away from their dad. Still, the oldest and youngest, two of their three daughters, were infected. Both children weathered the virus well. “We were fortunate,” says their dad.  Javier and his family Javier and his family A culture of care More than a year after the pandemic began, vaccinations and the careful of use of PPE (personal protective equipment, like masks) have imbued Martinez’s view from the front lines with a great deal of hope. In the early days, “there was a lot of uncertainty because it was brand new and we had to deal with a lot of changes. Provincial orders from the Chief Medical Officer of Health changed often, sometimes daily. One of the most dramatic shifts was the move to restrict visitors. That was really tough. Some of our residents have large families who are very close. I had to explain the health rules to many people and because these were mandated changes, we didn’t have much flexibility. This was very tough on residents and their families.” Careful adherence to the rules definitely kept people safe, says Martinez. Only one resident and a few staff at St. Marguerite Manor contracted COVID-19 in the first wave. The second wave was harder, but by then, something else was also at work. He says some residents talked openly about having lived good lives. They were not afraid to catch the virus and die. What they did not “want was to be the person who brought the virus into the manor. That care for other people was very strong.” Now that residents and most staff are fully vaccinated, life at the manor is more relaxed. Visitors are allowed in after screening and as of June 1, staff no longer have to wear face shields over their masks. “It’s amazing to see how things have changed for seniors in supportive living and long-term care because of the vaccinations,” says Martinez. Looking back, Martinez thinks about what the pandemic has taught him as a Catholic man, nurse, husband and father. He knows the people he works with were negatively impacted when denied access to family and friends. He also knows many of them weathered the storm with grace. “I guess I think about how we’re called to serve our neighbours—and to serve the best interests of our neighbours,” says Martinez. A parishioner at St. Gerard’s parish in Calgary, he also thinks about how the Catholic community supported that part of the gospel message. As he sees it, sometimes service is as simple as doing what’s best for others. Written by Joy Gregory for Faithfully
Photos courtesy of Javier Martinez Vanessa* carries something special with her every time she walks into the neonatal intensive care unit (NICU) at the Alberta Children’s Hospital. The NICU is where our city’s newest mortals, born early or with health problems, receive 24/7 care from teams of medical professionals, including Vanessa, a registered nurse. This is the kind of place where human beings routinely bear witness to some of the most powerful experiences life can offer. There, Vanessa has seen miracles happen. A faithful Catholic, she also knows that not every miracle ends with a baby carried home in the arms of loving parents. “You always pray for the best outcome, but it’s always in the hands of God.” So, what does Vanessa carry that fortifies her vocation to serve one of the city’s most medically-vulnerable populations? Faith and experience, says the cradle Catholic, wife and mother. In addition to her nurse’s training, this front-line worker recalls what it was like to be cared for as a child prone to severe asthma attacks that kept her away from school and off sports teams. She remembers how medical professionals, doctors and two cousins who were nurses, sometimes came to her family’s home in India, which lacked public health care. The visits kept her out of the hospital, keeping her well without great expense. They also gave Vanessa a lasting appreciation for what it feels like to be cared for during some of life’s weakest moments.
Written by Joy Gregory for Faithfully
 Lisza Bruder Lisza Bruder My life used to be crazy fast-paced. I was always filling my time, planning for the future, and writing out the steps I needed to follow to get where I wanted to go. Now, I don’t know what I will be able to do tomorrow or a week from now, never mind in a few years! This has been one of my biggest challenges living with chronic illness. Letting go of what I thought and hoped my life would be and accepting what it is. I had formed a large part of my identity around my ability to work hard. School was always hard for me, but through a lot of work I not only managed to successfully earn my PhD in biomolecular science, I was darn good at what I did. When my health made it clear I should switch careers, I moved into human services. My goal was to become a counselor so I did online courses towards a Masters program. As my health caused me to slow things down, I had to calm my stubborn and competitive sides and let go of this goal. With each step “backwards” I was very frustrated with the limitations I faced. However, I also found I preferred the little things to the big I had been pursuing. So I started an online business (Lisza’s Gifts) that allows me to use both the analytical and creative parts of my mind and might provide some long-term financial support as it grows. Through my many years of school I learned to ask questions and accept help. But I have discovered that it is not as easy to ask for help with personal things. My health is such that there are often days when showering is so exhausting I need to nap, so how am I supposed to clean my house? Or when I’m in a crazy amount of pain and I need my “good” painkillers but I can’t get up to get them, how am I supposed to prepare food? I knew that eventually my Crohn’s colitis and other conditions (both identified and those still under investigation), would leave me homebound, but in my early 30s? This was completely unexpected. Right now, my life seems to be all waiting. Waiting to get lab results. Waiting for the referral to yet another specialist. Waiting for more tests. Waiting in the ER. In these times of waiting, grace upon grace is granted. I receive help from family and friends to shovel snow, grocery shop, pick up prescriptions, drive me to and from appointments and the ER. I have the prayers of many people and the time to pray for them in return. I get to spend more time learning about my faith and myself. I have started to learn how to focus on what I need more than what I need to do. In 2020 my health went from inconvenient to unbearable. The worst part? The doctors do not know how to improve my situation. I don’t know why half my symptoms start or why some of them randomly stop. I either need to sleep a ridiculous amount or I get insomnia. If I’m lucky, I have 4 good days between my Crohn’s treatments every 4 weeks. I struggle with the loneliness and isolation; then I struggle with having patience with the people I do speak with. I believe that most people would say that I have more bad in my life than good, but I cannot control my circumstances. I can only control how I respond to them. It has been a steep learning curve to reach a place where I have largely accepted that my health will dictate more about my life than other factors. However, that doesn’t make it easy and I grieve every time. I think most of us learned in 2020 how we are less in control than we thought. I think the quote stating that we are all in the same storm, but in different boats applies well. There are things we can do to improve the ride even though we cannot change the storm, such as remembering that Christ is in the boat with each one of us.
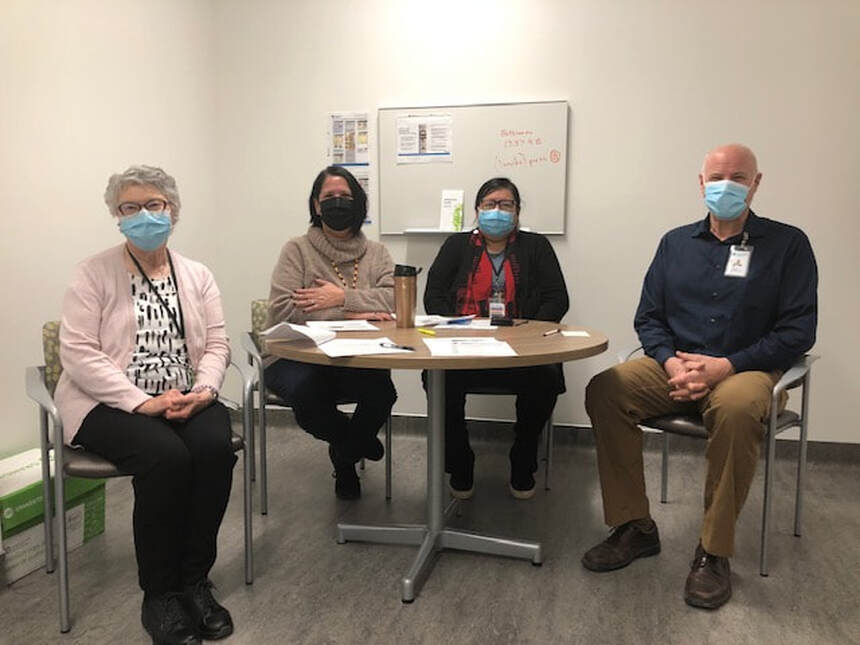
As COVID rages on we regularly see TV footage of health care professionals in hospitals. Yet barely visible is a small group of essential caregivers, often volunteers, who provide care for the soul, the Spiritual Care Teams. I recently met some of these caregivers inside the Chinook Regional Hospital (CRH) in Lethbridge. After navigating entrance protocol to rival a military base, I was met by Annella Wehlage, the Roman Catholic Spiritual Care Coordinator. She guided me to her office in a quiet section of the ‘tower’ office block. There I met John Moerman, the Hospital Chaplain, and the Indigenous Wellness Core, comprised of Sylvia Ann Fox/”Singing Alone From Above” (Traditional Wellness Coordinator) and Suzan Heavyshields (Indigenous Hospital Liaison). This small group explained how they work together to provided spiritual care needs to patients, and how COVID has changed what they do. Wehlage has been a volunteer since 2015 following a long career as a nurse. She outlined her daily routine which used to begin with a list of patients who designated a religious affinity on their admittance paperwork. She and the team would discuss a plan and then begin what Moerman referred to with a smile as ‘rounds’, or personal visits to each patient desiring spiritual care. However, COVID has changed all that. Now the imperative to prevent cross-contamination has reduced visitors to just one per patient, usually a family member. A second professional visitor is permitted in certain circumstances, e.g., a legal counsellor or a priest. And a limited number of additional visitors are permitted in end-of-life situations. So now the Spiritual Care Team can only visit a patient when specifically referred by family or nursing staff, or in an end-of-life situation. Wehlage is saddened by the loss of her four-person team of volunteer Eucharistic ministers who used to faithfully help her to bring the Eucharist to everyone who wanted it. Now Wehlage’s main responsibility is arranging for a priest to visit when requested. This she does with the help of a weekly roster and an ‘on-call’ list for weekends and evenings. There is always a priest available 24/7. The six priests on the list work tirelessly to bring the Sacrament of the Sick and the Sacrament of Reconciliation to patients, sometimes visiting the same person more than once. Their presence in the hospital is a blessing for more than just the patients. Not infrequently, a family member will also ask for a sacrament. The day I visited, Wehlage paused at a coffee kiosk in the hospital atrium where the barista told her how gratifying it was for her to simply see a parish priest walk by because her shift schedule made it impossible to attend Mass. Another uplifting aspect of Spiritual Care at CRH is how First Nation’s spirituality is often combined with Catholicism, for First Nations patients. Team member Fox explained, “Some people, their parents were strong Catholics and their grandparents were strong in our traditional ways.” So team members offer both forms of religious care concurrently. Moerman added, “That’s how God created us, with a traditional background, a family background, a cultural background, all together.” The CRH Spiritual Care Team and the Indigenous Wellness Core are clearly cohesive. “We’re friends outside of work”, Wehlage said, “We support one another.” They also work together to accomplish some extraordinary feats. Fox told of one gravely sick man whose wedding plans were interrupted by his illness. When she visited she found his fiancée present. She asked if there was anything she might help them with and they answered, “We’d like to get married this afternoon!” Fox and Wehlage executed a frenzy of arrangements from legal paperwork, securing a priest and arranging a special exemption for two family witnesses. Then they peeked in from the hallway to watch two people realize a dream that COVID couldn’t take from them. More commonly the teams deal with end-of-life situations. “Sometimes if patients get a difficult diagnosis nurses will request a spiritual care visit,” Wehlage said. She also makes a point of accompanying the priest in cases where the Sacrament of the Sick is administered, especially if it was requested by family members who aren’t permitted to visit due to COVID restrictions. “If a patient sees a priest arrive unannounced at their bedside, they may get scared,” Wehlage said. The teams have many times sat with a person during their final hours. Fox explained softly, “Nobody wants to be alone when they’re going.” When asked how else COVID has changed their work, the teams agreed that the hospital was much quieter with fewer visitors. That makes the teams’ work more important than ever. “Patient care can’t be done from home,” Moerman said. He added, “I don’t treat a patient with COVID any differently.” Nevertheless, additional precautions are necessary both at work and when returning home. Moerman said, “Early on I had a knot in my stomach, especially as my wife was baby-sitting our grandkids at home. I would put my clothes in the laundry as soon as I got home. I still do.” He admitted to turning off the news some days as well, “You have to limit COVID news or the fear can rise in you.” Wehlage spoke of baking as a stress-reliever and Fox had taken up traditional beading and making moccasins. Asked if they have a message for the readers of Faithfully, the teams had excellent suggestions. “Follow best practices, listen to the advice of professionals so we don’t overwhelm the 14-bed ICU at our hospital.” “If you know of somebody who’s Catholic and in hospital, notify their parish priest because the person might not have been at church for some time and their family might be too distracted to think of it.” “Check in with your extended family, just to talk, a wellness check.” It’s obvious that, both on and off the job, caring is deeply engrained in the nature of spiritual caregivers. Let us remember and pray for them in a special way this month.
Resources
"The celebration of the XXIX World Day of the Sick on 11 February 2021, the liturgical memorial of the Blessed Virgin Mary of Lourdes, is an opportunity to devote special attention to the sick and to those who provide them with assistance and care both in healthcare institutions and within families and communities. We think in particular of those who have suffered, and continue to suffer, the effects of the worldwide coronavirus pandemic." ~ Pope Francis. The theme of this year’s message is “You have but one teacher and you are all brothers" (Mt 23:8), which encourages a trust-based relationship with the sick and the nurturing of integral human healing. Please find here some resources for the World Day of the Sick (Feb. 11) this year:
Medical Assistance in Dying (MAiD) We would also like to direct your attention to the updated Bill C-7 webpage, and ask that you continue to pray and voice your concern on MAiD. "May our Lord both inspire and bring to accomplishment our efforts to embrace and protect the suffering and vulnerable, and to honour and uphold our rights and freedoms." ~ AB & NWT Bishops See webpage
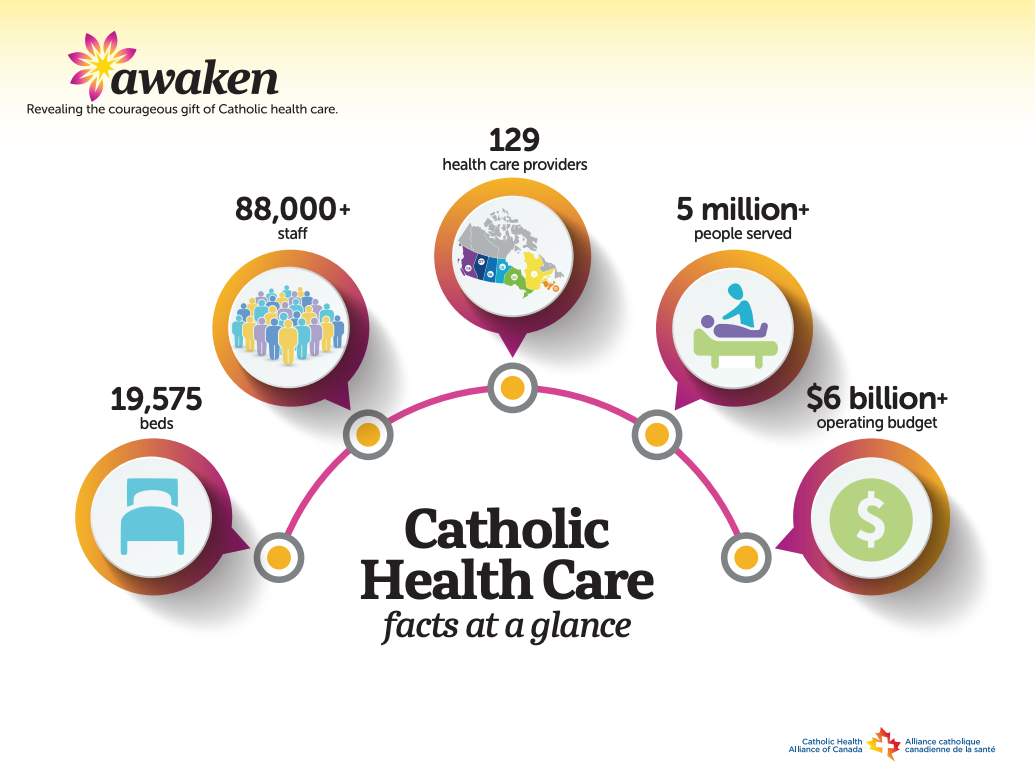
At the heart of Catholic health care is a deep respect for the intrinsic value and dignity of every human being and an unwavering commitment to serving all people, from all backgrounds and faiths – especially society’s most vulnerable.
This week is the National Health Care Week (Oct 4-10) - we invite you to learn more about National Catholic Health Care by visiting Catholic Health Alliance of Canada Download:
This is a time for us to reflect and give thanks for the gift of Catholic health care, and for the thousands of dedicated staff, physicians and volunteers who care for those in need. Like the Sisters who came before us, the Covenant family is united by a shared mission that calls on us to serve people from all backgrounds and society’s most vulnerable, according to our values. During National Catholic Health Care Week, let us give thanks for the courageous gift of Catholic health care during these challenging times—in hospitals, community health centres, or seniors care homes. We pray:
Catholics across the Diocese of Calgary are looking for ways to de-stress from the distress. Adjusting to the new normal foisted on the global community by COVID-19, a disease that didn’t even have a name just weeks ago, thousands are live-streaming daily and Sunday masses. Others turn to traditional Catholic prayers like the rosary and Divine Mercy chaplet, seeking grace for the dead, the sick, their families and caregivers. Sr. Donna Marie Perry, FCJ, knows the news is bad. But the Calgary-based social worker and psychotherapist wants people to remember that the steps we take to stay “physically healthy should also include a focus on our mental and spiritual well-being.” That earns a quick nod from Dr. Peter Doherty, an associate professor of psychology and family studies at St. Mary’s University in Calgary. Dr. Doherty, whose work focuses on the integration of psychology and spirituality, agrees people should take mental health issues seriously in times of crisis. Mental health matters Sr. Perry is the clinical director of Insight Counselling and Therapy Centre. This not-for-profit offers long-term counselling at sliding rates as low as $5 a visit. Insight delivers care through practicum students supervised by Sr. Perry. All of the students are finishing master of counselling programs with various universities. The organization is one of the community-based organizations that benefits from Together in Action, an annual fundraising campaign by the Roman Catholic Diocese of Calgary. Given the imperatives of “social distancing” during the pandemic, Insight’s students currently offer support via phone. Sr. Perry herself lives in a seniors’ residence with strict pandemic protocols. With St. Mary’s University shuttered, Dr. Doherty is also staying close to home. They offered readers of Faithfully some ideas about how to make mental health a priority in trying times. Stay informed. Make healthy choices. “Fear is a healthy response to the situation, and it makes sense to stay informed. But let’s be smart about how much news we watch and read,” says Sr. Perry. She recommends people listen to morning updates and check in again in the afternoon or evening. A 24-hour news cycle includes a lot of recycled information and “when you’re hearing the same news all the time that increases stress,” says Sr. Perry. Hoarding items as basic as toilet paper shows “an emotional response to the crisis that doesn’t make rational sense,” adds Dr. Doherty. He also shakes his head when he sees examples of people not following recommendations for safe social interaction. One of the healthiest ideas he’s seen to date suggests people “not act as if you’re afraid of getting the virus. Instead, act as if you are trying to protect other people from getting it. The best information we have says most people who get this virus will survive. But we need to protect those who are vulnerable.” People who follow that advice should take mental comfort in knowing they are doing the right thing, says Dr. Doherty. Strengthen family ties. The social distancing protocols recommended by public health officials isolate family units. Sr. Perry’s urges families to use the time to your family’s advantage. Play games. Share meals. Go for walks where you can be 2 m from other people. If you have a backyard, use it. Reach out. “It’s like we are disconnected, together,” says Dr. Doherty. Since our own mental health benefits when we interact with others, this is a good time to phone, text, email, FaceTime or Skype with people we haven’t heard from in a while, “especially if we know people who might be alone.” This is also a good time to reach out to people whom we’ve hurt and vice versa. The words, “I forgive you,” are a way to free ourselves from the heavy, energy-sapping emotional burdens we carry when we haven’t let go of real or imagined hurts, says Dr. Doherty. This kind of pain bleeds into how we interact with others and how we handle strife. “It can keep us from handling unrelated situations well.” Pray. Pray together. Dr. Doherty encourages people of faith to use prayer as a conduit to deeper conversion. When we pray for the isolated, for those who’ve lost jobs and for people on the front lines of health care, prayer becomes a way to reach past ourselves to Christ, says Dr. Doherty. This can be helpful for people who grieve the fact that they cannot attend mass to receive the Eucharist. Family prayer is also helpful, says Sr. Perry. Praying for others teaches children that prayer is a way of helping others—and it reminds adults of the same thing. “It’s really important not to get caught up in ‘self’ and to keep looking outward,” says Sr. Perry. “Prayer can be very relaxing, too,” notes Sr. Perry. Following the Jesuit tradition of her charism, she uses her evening prayers “to look back on the day, to think about what went well and what didn’t go as well and to give thanks to God for the day.” She’s added more Hail Marys to her day by reciting that prayer while she lathers her soapy hands for the requisite 20 seconds (as recommended by public health), prior to rinsing off the soap with water. Sr. Perry says the Hail Mary is a good replacement for singing the ABCs or Happy Birthday songs. Listen. Talk. Be kind. People manage stress differently. If you see more anger than you’re used to, remember that unresolved fear may be expressed as anger, explains Sr. Perry. She encourages parents to listen when their kids talk about their fears. Be open to their questions and offer age-appropriate responses. “Let them know that you don’t know everything, but you will figure it out together.” Also, remember that children internalize messages from the external world and believe that everything that happens relates to them. It’s a matter of maturity, not selfishness, says Sr. Perry. “Children internalize information to make sense of their environment with limited experience. They use that information to make decisions about themselves and the world. They build what we call a script, and we live out of those childhood beliefs.” Laugh often. Love much. With so much doom and gloom, Sr. Perry suggests people who are feeling sad work some comedy into their screen time. She and Dr. Doherty admit they are especially worried about individuals and families who did not go into the current pandemic in strong mental health. “Not all families are healthy,” says Sr. Perry. She urges people who see others struggling to reach out with kindness. Where appropriate, you can also recommend they access support from community-based organizations. ===== Calgary Distress Centre Helpline: 403-266-HELP (4357) Written by Joy Gregory for Faithfully
Photo: Lightstock
The 28th World Day of the Sick was celebrated on February 11, 2020. Saint John Paul II initiated the World Day of the Sick to encourage the faithful to pray for those who suffer from illnesses and for those who care for and minister to them. February 11 is also the Optional Memorial for Our Lady of Lourdes. In 1858, the Blessed Virgin Mary appeared many times to St. Bernadette in the hollow of the rock at Lourdes. Since then, there have been many miraculous cures and conversions attributed to the intercession of the Blessed Virgin Mary at Lourdes. The Roman Catholic Church has a long history of founding and engaging in the provision of healthcare rooted in a faithful response to the Gospel call. “After this the Lord appointed seventy others … Whenever you enter a town and its people welcome you, eat what is set before you; cure the sick who are there, and say to them, ‘The kingdom of God has come near to you.’” (Luke 10: 1, 8-9.) The Catechism of the Catholic Church (CCC) reiterates this call and says, "Heal the sick!" The Church has received this charge from the Lord and strives to carry it out by taking care of the sick as well as by accompanying them with her prayer of intercession. She believes in the life-giving presence of Christ, the physician of souls and bodies.” (CCC, 1509.) The Pastoral Letter for Catholic Health Care issued by the Canadian Conference of Catholic Bishops offers eight guiding principles:
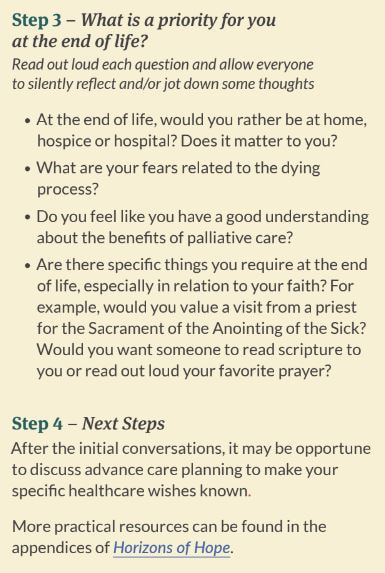
Throughout Canada’s history, many women and men, clergy, religious and lay, have dedicated themselves to living out these principles by providing medical and spiritual care for the sick. In Alberta, communities of religious women founded the provincial hospital system and delivered quality healthcare with a preferential option for the poor. The first hospital in this province was established in 1863 by the Sisters of Charity (Grey Nuns) in St. Albert. The founding of the hospitals spread from this beginning and fostered the hospital system we enjoy today. We are all indebted to this rich legacy of faith, fortitude, perseverance and care of the sick. Pope Francis’ Message for the World Day of the Sick, “Come to me, all you who labour and are burdened, and I will give you rest” (Mt 11:28), offers comfort to the sick saying “brothers and sisters who are ill, your sickness makes you in a particular way one of those “who labour and are burdened”, and thus attract the eyes and heart of Jesus. In him, you will find light to brighten your darkest moments and hope to soothe your distress.” Pope Francis also offers timely encouragement to healthcare providers, “may you always strive to promote the dignity and life of each person, and reject any compromise in the direction of euthanasia, assisted suicide or suppression of life, even in the case of terminal illness. I echo Pope Francis’ message and encourage healthcare providers “to be consistent with your “yes” to life and to the human person. Your professionalism, sustained by Christian charity, will be the best service you can offer for the safeguarding of the truest human right, the right to life.” My hope is that our society – and each of us – will better recognize the profound human-ness of the tremendously important phase of life that we know as ‘end of life’ or palliative. It might seem to be normal to fear this time, and perhaps to seek to avoid the experience of living when dying is inevitable due to an illness. While we understand as compassionate humans the natural grief and concern that accompanies the possibility of dying, there are other ways to experience it – and I have seen these other ways in countless individuals. Those people have taught me that the time prior to their natural deaths can be a time of growth, of healing of relationships, of seeking and giving forgiveness, of preparation of hearts and souls for meeting their God, of internal reflection and openness, of teaching those around them through their example, even a time of profound peace and joy, and certainly a time of giving love unreservedly, and of accepting loving care from others while vulnerable and frail. Society’s response to suffering is to enact a law that allows physicians and nurse practitioners to deliberately end a person’s life through the provision of chemicals that are specifically meant to cause death. But suffering - whether physical, mental or emotional - can and should be a trigger for our spiritual and human selves to respond differently based on compassion. All of us can protect and support those who are particularly vulnerable and who might otherwise choose assisted death as a way to stop their suffering because they cannot access society’s resources due to their vulnerability. We should not be afraid to support conscience rights for people in medical professions. We want people who are engaged in challenging health care tasks to be able to honour moral commitments for at least two reasons: a) so that they are not morally harmed by being forced to do things against their conscience; and b) so that they can do their best work for all the people they care for, by being whole to the deepest parts of their beings. Since conscience rights are not absolute rights that prevail in all circumstances, supporting conscience rights can be done without impairing patient access to needed services. Those of us who are able to, have a duty to advocate with decision-makers to minimize the harms of assisted death and to reject the further expansion of the criteria for assisted death eligibility. We must do what we can to promote widespread availability of expert end of life care. The focus of this care is to reduce suffering from symptoms and also to assist people to live as well as they can as they approach the end of their natural lives. Palliative, end of life care has been so positive and helpful for so many people and simply should be universally available. The very human act of dying and of preparing for death while we live demands a response that does not seek first to snuff out life, but rather that brings out our love for each other and communal support while we acknowledge the human conditions of frailty, vulnerability, uncertainty and eternal Hope. Written by Dr. Eric Wasylenko, a palliative care physician and clinical ethicist. The Bishop’s of Alberta and Northwest Territories have written a pastoral letter on the proposed expansion of Medical Assistance in Dying (MAiD). They encourage Catholics to write a letter to their members of parliament to share their opposition to euthanasia/assisted suicide.
“Pilgrimage, Sanctuary and Peace in the Parks”: A research snapshot and public talk on parks and nature at the end of life. We all feel it – whether looking outside, in a field, at a beach, or on a mountain – nature gives us perspective about life and death. There is growing evidence of how natural environments impact our physical, mental and spiritual well-being. Little is known, however, about the place of parks and nature at the end of life, or the impact of parks and nature on quality of life during palliative care or in grief and loss…until now! A recent 2018 study discovered that experiencing “Peace in the Parks” was an opportunity for: Personal Exploration, Social Discovery and Institutional Transformation. Despite the challenges to get to parks and natural places, it was always “worth it.” Even brief opportunities were an opportunity to “park palliative care”, and to have sanctuary from the stream of appointments and persistent identity as a “dying patient” or “caregiver.” Research participants shared, “here [in the park] we can just be ourselves”. The experiences were both calming and energizing – providing patients and family members a sense of their strength and the courage to take other journeys they had been previously cautious about undertaking. Everyone can make the connection with nature. Ultimately there is value in even parking or sitting in areas with views of nature or short walks or strolls with a stretcher or adaptive equipment. Access does take planning, information and communication, and the research team discovered that supporting access to parks and nature for those in palliative care and caregivers is not a call for a new program per se, but rather an invitation, and a mindset that can be influenced by training, information and coordination of services. Further program and study is underway now to extend and expand the discoveries made – the pilgrimage and the pursuit of sanctuary continues. By Dr. Sonya Jakubec
======= To learn more about Parks & Nature at the End of Life, to hear the stories and to be inspired by the pilgrimage of palliative patients and caregivers to Alberta Parks, join Dr. Sonya Jakubec (MRU) and co-researcher Jennell Rempel (Alberta Parks) for a free public talk and short documentary film screening with the Calgary Public Library on Thursday Jan 23, 2020 from noon to 1:30 pm at the Central Library’s Patricia A. Whelan Performance Hall. Fr. Michael Storey knows he might not be able to attend a formal Remembrance Day service this November 11. As a hospital chaplain in the Diocese of Calgary, the Catholic priest could find himself beside a hospital bed when other Calgarians pause in reverent silence at the 11th hour of the 11th day of the 11th month. But make no mistake. While Fr. Storey may not be able to hear the dying notes of the Last Post, he will feel the lament in his heart. And he will remember. November 11, for this priest, is a matter of country, family and faith. Fr. Storey’s dad and brother served the Canadian navy in the Second World War. During the same conflict, where 42,000 Canadians died and another 55,000 were wounded, his uncles were soldiers in the Canadian Armed Forces (CAF). Having grown up in a family that sacrificed so much for so many, Fr. Storey admits it wasn’t difficult to step up when a friend and Calgary-based reservist mentioned the need for a military chaplain in Calgary. “I realized that military personnel needed spiritual support. I was also working at St. James parish, so it was easy for me to go back and forth between the parish and Currie Barracks.” Fr. Storey served that role in Calgary from 1987 to 1999. Fr. Sajo Jacob, parish priest at Mother Teresa Syro Malabar Church in Calgary, assumed the military chaplaincy about two years ago. He was introduced to the ministry by students he met while serving as the campus chaplain at SAIT and Mount Royal University, a role he held from 2009 to 2019. Some of the students he met there joined the military and invited Fr. Jacob to bring his ministry there. Two years into the role, he’s grateful for the chance to serve military personnel, many of them young people, as they encounter the challenges of military service in defense of the country. “They are often away from their homes, they face personal crisis, they sacrifice for the country and people, and I felt a calling that I will be able to help them.” A ministry of presence Unlike more typical priestly ministries which focus on bringing sacraments to the faithful, military chaplaincy is a “ministry of presence.” As a chaplain, Fr. Storey met military personnel at formal events. He also dropped by places like a military rifle range if he knew soldiers and reservists were there to practise. “You do what you can to remind them that you are there if they need you,” he explains. His formal role also included being one of two uniformed military officers who made next-of-kin calls to the families of military personnel who died in service to their country. “I was on three of those calls during my 12 years in the service. It was humbling,” he recalls. The chaplain’s role is akin to “being a guide and mentor,” adds Fr. Jacob. “Sometimes you become a point of contact at a time of crisis and challenges. It is a vocation where you journey with people and you become God’s instrument to share peace and love.” Whereas parish priests serve Catholic congregations, campus and military chaplains work in secular and interfaith spaces. “Chaplains are there for everyone and we guide and support whoever seeks help, regardless of religion, or orientation,” explains Fr. Jacob. His faithful presence in personal crises has included talking to people contemplating suicide. There is no question that military chaplains witness Christ for others, adds Fr. Storey. He remembers being touched by the words of a former altar boy who attended an event to commemorate the priest’s 40th anniversary in the priesthood. “He told me, ‘I was so proud of my parish priest when I saw him in his uniform,’ That meant a lot to me.” He and Fr. Jacob both view military chaplaincy as service to their nation. “It is my role in the nation-building process,” explains Fr. Jacob, himself an immigrant from India. In addition to serving military personnel as a spiritual guide and mentor, Fr. Jacob helps organize religious services and advises commanding officers in matters of religious accommodations and spiritual and ethical issues. This Remembrance Day, Fr. Jacob will officiate at a November 11 ceremony. He says the events do more than remember fallen soldiers and veterans, they also inspire young Canadians in their message of service. Written by Joy Gregory for Faithfully
|
Author
Catholic Pastoral Centre Staff and Guest Writers Archives
July 2024
Categories
All
|






























 RSS Feed
RSS Feed